📡Understanding Digital Divide in Healthcare
Your ZIP code (location) determines your ease of access to quality healthcare. But soon the determining factor will be your IP address.
Two things you’ll get from TWIP today…
As healthcare providers today increasingly turn to technology like telehealth solutions and chatbots, the needs of those who are not online or tech-savvy are neglected. This creates Digital Divide, which we explore in TWIP today.
Video: The story of Glocal Healthcare System - digital Inclusion done right.
👁️Digital Divide in Healthcare: Reaching the Unreached
In India, approximately three-quarters of our 1.4 billion population live in rural areas, yet over 75% of health care infrastructure is concentrated in metro cities🌆. Practically, the ZIP code of the citizens determines their access to healthcare. But soon the determining factor will be their IP address, or the lack thereof.
As healthcare providers today increasingly turn to technology like telehealth solutions and chatbots🤖 to improve care delivery and prevent staff burnout, we neglect the needs of those who are not online or tech-savvy. Technology that’s meant to democratize healthcare access is now in a way creating more disparity.
This leads to digital divide in healthcare.
According to a recent research published by Info-Tech Research Group, "While affluent communities and urban centers typically benefit from seamless access to digital health resources, rural populations are often left behind. Even in urban areas, digital divide is apparent in populations impacted due to racial, ethnic, financial, and other socioeconomic barriers."
📰This Week in Products we explore the the problems leading to digital divide and raise questions that leaders should ask themselves to build products and businesses that minimize digital divide and promote health equity.
💡Let’s first understand the impact of digital divide
As product leaders, we need to understand that the digital divide in healthcare isn't just a technological problem; it's a societal one. It has far-reaching implications:
❌Limited access to care: Telehealth, remote patient monitoring, and other digital health services can be inaccessible for those without reliable internet or devices.
💔Exacerbated health disparities: Those who lack access to digital health tools are more likely to suffer from chronic diseases and have poorer health outcomes as more healthcare providers opt for digital treatment pathways.
💸Increases healthcare costs: The lack of digital tools can lead to inefficient care delivery and higher costs for patients and providers.
We have a unique opportunity to create solutions that can bridge this gap and ensure equitable access to healthcare for all. So, what are the problems and areas of opportunity?
🚧Barriers Leading to Digital Divide in Healthcare
1. Internet access and gender disparity🌐
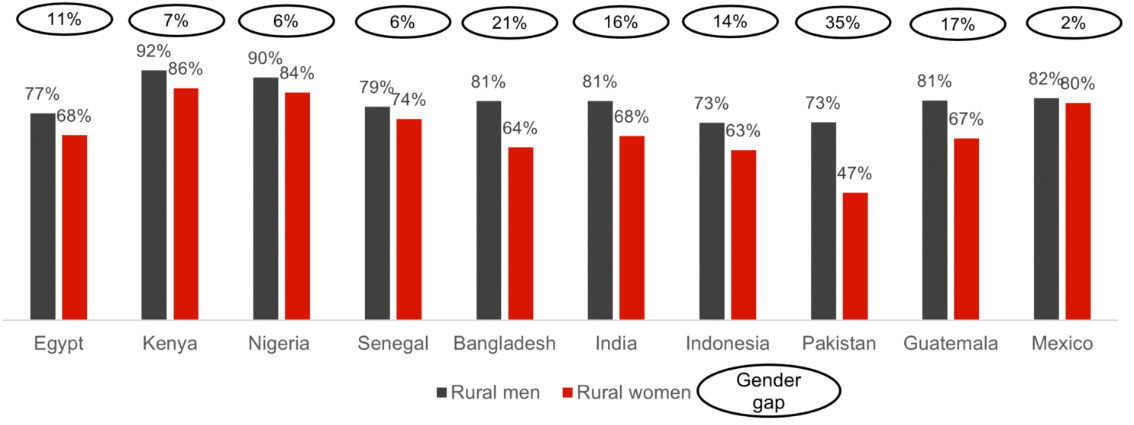
Weak network coverage and lack of IT infrastructure are key barriers to digital transformation in the health sector. According to DataReportal’s Digital 2024: India report, India’s internet penetration was 52.4 % (751.5 million internet users) at the start of 2024.
However, this figure masks significant gender disparities. According to National Family Health Survey (NFHS) 2019-21 only 57.1% of males and a mere 33.3 percent of females have ever used the internet in India!
Here’s a Question to product leaders💭- How can you ensure access to digital health solutions to people that have limited or no access to internet, especially among rural females?
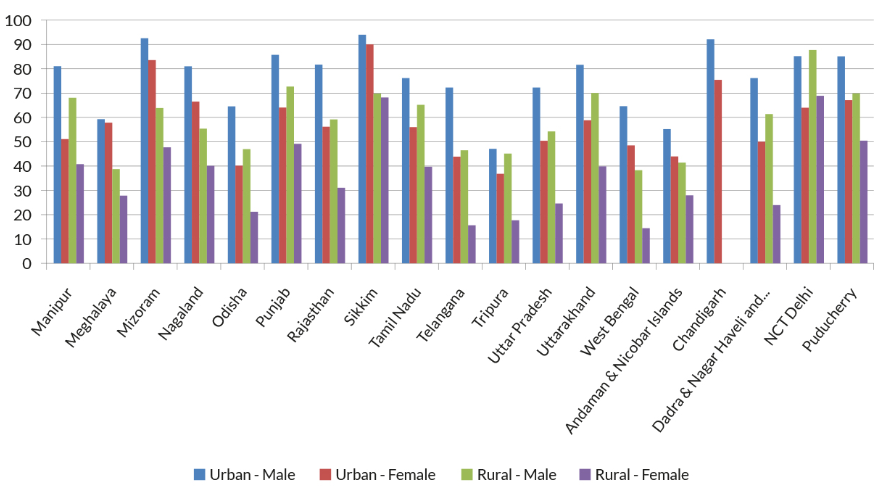
2. Smartphones & PC penetration📱
Relatedly, a lack of basic digital infrastructures, such as access to smartphones or computers is also a major barrier. While mobile ownership has grown considerably in India, rural-urban disparities in mobile ownership are very telling - a higher percentage of urban women own mobile phones compared to rural women.
Age and caste groups further contribute to the digital divide in mobile ownership. In this context, patients resort to using their family members’ smartphones or rely on more digitally savvy kith and kin to access any form of digital services.
Question to leaders💭- How can you ensure the adoption of your digital health solutions among users who do not have a smartphone or are not digitally savvy? Remember, these users rely more on their digitally savvy kith and kin to access any form of digital services.
3. Operational costs💸 and complexity of digital health solutions
A recent study revealed that poor health literacy (81%), financial burden (75%), lack of technology/availability of resources (58%) and lack of expertise (53%), are the predominant barriers to smartphone-based telerehabilitation care programs for patients with Chronic Obstructive Pulmonary Disease. It holds true for any other disease as well.
Especially for smaller healthcare providers, financial concern is a barrier to implement digital transformation in healthcare. Concerns about the complexity and ongoing cost of maintaining digital hospital systems like HMS, EHRs, and mHealth platforms are there.
The cost-complexity issue is compounded by a lack of technological expertise among healthcare professionals🧑⚕️. Ambiguity on the return on investment of expensive digital technology also prevails among healthcare institutions.
Questions to product leaders💭: How can you your solutions increase digital health adoption among healthcare providers by cutting down costs and making it easy for the non-tech savvy?
Also, how can you effectively add more value to the digital health solution, and at the same time convey the value propositios in a better way?
4. Mental Roadblocks🤔 - Preference for in-person consultation
A mixed-methods study on 1226 patients revealed that 71% patients preferred in-person visits, while only 29% preferred telemedicine. The elderly especially prefer face‑to‑face consultations and remain skeptical about seeking healthcare online. Factors such as education level, specific health conditions, and prior experience with telemedicine too influenced the preference for digital healthcare solutions.
Doctors too aren’t entirely convinced about digital health solutions, despite reports of remote GP appointments being as effective as in-person care. From what I’ve seen, clinicians exhibit a bit of technofobia - an inherent fear of misdiagnosis despite advancements in remote medical diagnostic processes & systems.
So, the question in my mind is: are the clinicians avoiding technology based on the evaluation of the empirical research? Or, is it based of their own worries about using digital health solutions? How do we address the trust issue?
Questions to product leaders💭: How can you reduce the fear of digital health systems and showcase its prowess, not just to patients, but also among healthcare professionals?
5. Usage barriers🚫
Several barriers, deeply rooted in socio-cultural and linguistic factors, continue to impede the widespread use of digital health tools by by patients.
🗣️Language Barriers and Accessibility:
India is a linguistically diverse country, with over 1,600 languages spoken. Yet, the majority of digital health platforms are predominantly available in English or Hindi, limiting access for the rest.
This linguistic gap can be particularly challenging for older adults and those with limited education, who may find it difficult to navigate complex digital interfaces, let alone comprehend medical jargon.
Question to leaders💭 - How can you ensure that your digital health solutions are accessible to non-English speaking populations? Are there ways to incorporate regional languages, visual aids, and voice-based assistance to make digital health platforms more inclusive?
📚Digital Literacy and Usability:
Even when language is not a barrier, the level of digital literacy varies widely across different demographic groups. While younger, tech-savvy users may easily adapt to telehealth apps and platforms, older adults or those with lower educational backgrounds may struggle. The design and user experience of these platforms often assume a certain level of digital competence, which is not universally present.
Question to leaders💭 - How can you design your digital health solutions to be intuitive and user-friendly for all, regardless of their digital literacy levels? What role can community-based training and support play in enhancing digital literacy and encouraging the adoption of these solutions?
🛡️Cultural Sensitivity and Trust:
Beyond language and literacy, cultural factors play a significant role in healthcare. Many patients may have ingrained beliefs and practices that influence their acceptance of digital health services. For instance, the preference for in-person consultations we talked about earlier is often driven by trust in the personal touch of a healthcare provider, which digital interfaces may lack.
Additionally, the fear of data breaches or misuse of personal information can also deter patients from embracing digital health solutions.
Question to leaders💭 - How can you build cultural sensitivity into your digital health solutions? What measures can you take to build trust and reassure patients that their data is secure and their cultural needs are respected?
🗣️Effective Communication and Patient Engagement:
Communication is the cornerstone of effective healthcare. In a digital environment, ensuring clear and empathetic communication between patients and healthcare providers becomes even more crucial.
Miscommunication can lead to misunderstandings, mistrust, and ultimately, poor health outcomes. Moreover, the lack of physical presence in digital interactions can make it harder to build rapport and engage patients in their healthcare journey.
Question to leaders💭 - How can you enhance communication in digital health platforms to ensure that patients feel heard, understood, and engaged? Are there innovative ways to integrate human elements into digital interactions to foster stronger patient-provider relationships?
🛠️The Role of Product Leaders in bridging digital divide
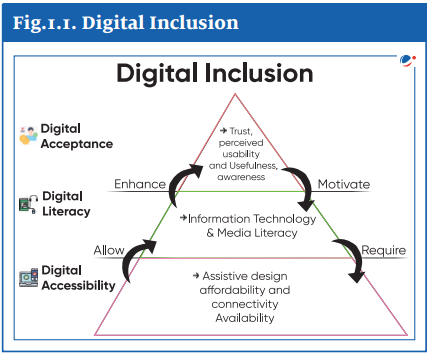
If you look at the questions listed above, it all boils down to three things which are the basis of digital inclusion for any product: Providing digital accessibility, digital literacy, and digital acceptance.
Founders and product leaders have a unique opportunity to tap into the huge TAM of digitally un-accessible masses (so far) by solving the problem of digital divide by building digitally inclusive and equitable solutions.
The growth of digital financial services, including the UPI and allied apps in every nook and corner of India, is a great example here. Now, you have the chance to build and be part of the UPI moment for healthcare.
Key Strategies for Bringing Digital Inclusion
Personalized Solutions:
Tailored interfaces: Design interfaces and system that cater to diverse cultural backgrounds, language preferences, and literacy levels.
Adaptive content: Use AI to personalize health information and recommendations based on individual needs and preferences.
Affordable and Accessible Technology:
Low-cost devices: Partner with organizations to provide subsidized health systems. Look for a offline + online models to bridge digital divide.
Subscription models: For smaller healthcare providers, offer flexible subscription plans for digital health services to make them more accessible.
Digital Literacy Training:
Interactive tutorials: Develop easy-to-follow tutorials and resources that teach users how to use digital health tools effectively.
Community-based programs: Partner with community organizations to offer digital literacy training sessions.
Enhanced Technical Support:
24/7 support: Provide round-the-clock technical support channels, including traditional phone support.
Remote troubleshooting: Offer remote assistance to help users resolve technical issues.
Data Privacy and Security:
Robust security measures: Implement strong security measures to protect user data.
Transparent data practices: Clearly communicate how user data is collected, stored, and used.
Digital divide in healthcare is a complex issue, but it's one that we can address.
While digital transformation in the health sector is inevitable, effective sustainability relies on various factors that influence its implementation. That’s where the products we build play a significant role.
By working together, product leaders, healthcare providers, and policymakers can create a more equitable and accessible healthcare system for everyone, that reduces digital divide.
You might also be interested in…
Digital Inclusion done right - Story of Glocal Healthcare System
In this video, Dr Sabahat S Azim, discusses the challenges of healthcare access in rural and underserved areas of India and how his company, Glocal Healthcare, is using technology to bridge the gap.
Through telemedicine, a clinical decision support system, and the use of medical devices connected via the Internet of Things, Glocal Healthcare aims to provide efficient and affordable primary healthcare to all.
They have also developed small, portable clinics called hello life cx that can be installed anywhere for just four dollars, offering primary consultations, medication, and investigations. These clinics have increased healthcare equity in society and are helping to reduce poverty by providing accessible healthcare to all.
I hope you enjoyed this week's curated stories and resources. Check your inbox again next week, or read previous editions of this newsletter for more insights. To get instant updates, connect with me on LinkedIn.
Cheers!
Khuze Siam
Founder: Siam Computing & ProdWrks